Why Prednisolone is used in nephrotic syndrome
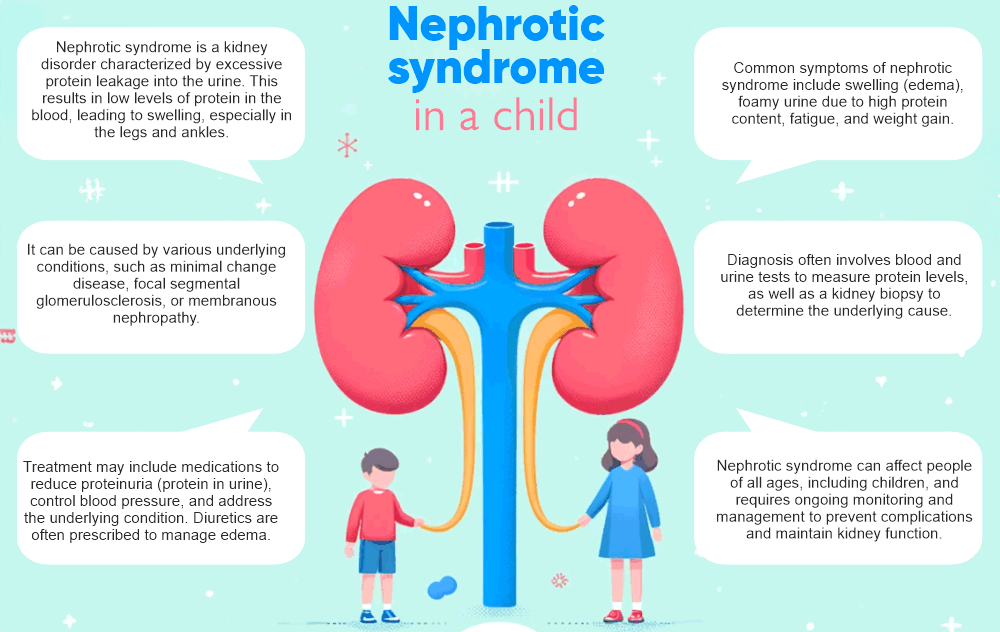
Nephrotic syndrome in a child
Steroid-Sensitive Nephrotic Syndrome is a medical condition characterised by the sensitivity of the kidneys to steroids.
Steroid-Sensitive Nephrotic Syndrome (SSNS) is a paediatric kidney illness. It is distinguished by proteinuria, edema, and elevated levels of cholesterol. SSNS is classified as steroid-sensitive due to its high responsiveness to corticosteroid therapy, which effectively reduces proteinuria and enhances renal function. The precise aetiology of SSNS remains unknown, but it is hypothesised to be associated with an aberrant immunological response and genetic predisposition. Social stigma and negative stereotypes (SSNS) can profoundly influence a child’s overall well-being and necessitate vigilant supervision and intervention from a healthcare team. Gaining a comprehensive understanding of the concept of SSNS is of utmost importance in order to promptly identify, effectively handle, and enhance the results for children who are impacted by this condition.
Incidence of Steroid-Sensitive Nephrotic Syndrome in Childhood
Steroid-sensitive nephrotic syndrome (SSNS) is a prevalent renal condition in childhood, affecting roughly 2-7 occurrences per 100,000 children. Approximately 30-50% of children diagnosed with SSNS are expected to develop frequently relapsing nephrotic syndrome (FRNS), characterised by the occurrence of many relapses over a period of time. Nevertheless, research has demonstrated that the implementation of prednisone medication can substantially diminish the likelihood of recurrence in children diagnosed with SSNS.
Studies investigating the length of prednisone treatment in children’s initial episode of SSNS indicate that extended treatment durations may reduce the likelihood of developing FRNS. For example, a study discovered that a longer initial course of prednisone medication (lasting 16 weeks or more) was linked to a reduced incidence of FRNS in comparison to a shorter term of treatment.
Moreover, using prednisone on a daily basis during viral infections has demonstrated potential advantages in reducing recurrence when compared to the use of prednisone every other day. Implementing this strategy may effectively decrease the occurrence of relapses and enhance the overall control of steroid-sensitive nephrotic syndrome (SSNS) in paediatric patients.
To summarise, SSNS is a common illness in kids, and the administration of prednisone medication can significantly contribute to mitigating the likelihood of often recurring nephrotic syndrome. Furthermore, administering a much extended course of prednisone at the beginning of treatment and maintaining a daily prednisone regimen throughout viral infections may provide supplementary advantages in preventing relapses in children with SSNS.
Factors that increase the likelihood of developing SSNS
Steroid-sensitive nephrotic syndrome (SSNS) is a medical disorder characterised by the presence of nephrotic syndrome and a positive response to treatment with corticosteroids. The risk factors associated with the development of SSNS include genetic susceptibility, viral infections, allergies, and exposure to environmental pollutants. Furthermore, research has demonstrated that the length of time prednisone is used and the timing of its administration during infections can influence the likelihood of frequently relapsing nephrotic syndrome (FRNS). Extended use of prednisone has been correlated with an elevated susceptibility to developing frequent relapsing nephrotic syndrome (FRNS), whereas the use of prednisone during infections has been connected with a greater probability of recurrence.
Allocation concealment and attrition bias are crucial factors in pertinent research. Research that lacks proper allocation concealment can lead to selection bias, whereas attrition bias can arise when there is a disproportionate loss of participants in the treatment and control groups. Hence, it is imperative for researchers to guarantee appropriate allocation concealment and reduce attrition bias in order to precisely evaluate the influence of prednisone medication on the likelihood of developing FRNS in patients with SSNS.
Commencement of Prednisolone Therapy
Prednisolone is a frequently given corticosteroid drug that is utilised to diminish inflammation and inhibit the immune system. It is frequently recommended for a broad spectrum of ailments, such as asthma, allergies, arthritis, and autoimmune disorders. The initial administration of prednisolone usually entails a greater dosage to promptly alleviate the inflammation, succeeded by a progressive reduction in dosage through a tapering plan to mitigate any potential side effects. It is crucial to adhere strictly to the recommended dosage and gradual reduction plan while remaining vigilant for possible adverse reactions. Comprehending the initial treatment strategy and correctly adhering to the administration of prednisolone is crucial for effectively controlling the underlying disease and guaranteeing optimal results.
Treatment Objectives
The main objective of treatment is to evaluate the efficacy of interventions in attaining favourable health outcomes. When doing the analysis, we utilise measures of treatment effect such as risk ratios for binary outcomes and mean difference or standardised mean difference for continuous scales to address these objectives.
Risk ratios are computed for binary outcomes in order to compare the likelihood of an event happening in the treatment and control groups. StandardizedThe mean difference is a metric used to quantify the average disparity in continuous scale outcomes between different groups. On the other hand, the standardised mean difference accounts for the variability of the measurements.
Nevertheless, the analysis did not incorporate the time to relapse to avoid potential data bias. The duration before relapse can be affected by multiple factors, including patient compliance, therapy adherence, and follow-up care, potentially resulting in biassed outcomes. To mitigate potential biases and enhance the precision of the study, it was decided to eliminate the time to relapse as a metric for evaluating the effectiveness of the treatment.
Ultimately, through the utilisation of suitable indicators of treatment impact and mitigating any distortions in the data, the study seeks to offer a lucid comprehension of the efficacy of therapies in attaining the intended health results.
Administration and Length of Treatment
The study compared the efficacy of high dose oral methylprednisolone therapy with normal prednisone therapy in patients experiencing acute asthma exacerbation. The dosage and duration of medication were as follows:
In the high dose oral methylprednisolone group, patients received a daily dosage of 125 mg of methylprednisolone for a duration of 3 days, followed by a daily dosage of 40 mg of prednisone for a duration of 11 days. This was in contrast to the conventional prednisone group, who were administered a daily dose of 40 mg of prednisone for a duration of 14 days.
In a separate investigation investigating the utilisation of prednisone in individuals with rheumatoid arthritis, the amount and length of treatment differed according on the seriousness of the ailment. Patients exhibiting minor symptoms were administered a daily dosage of 5-10 mg of prednisone for a brief period. Conversely, patients experiencing moderate to severe symptoms were prescribed higher dosages for an extended duration, often commencing at 10 mg and subsequently reducing over a span of several weeks to months.
In general, the prescribed amount and length of prednisone treatment can differ based on the particular medical condition and the seriousness of symptoms, whereas methylprednisolone may be employed as a substitute in certain instances. Healthcare practitioners must take into account specific patient circumstances when deciding on the optimal dosage and duration of medication.
Negative Consequences of Prednisolone
Prednisolone, a corticosteroid drug, can cause many detrimental consequences on the body. An important detrimental consequence is its influence on blood glucose levels, which might result in hyperglycemia in certain people. This is especially worrisome for persons who have diabetes or those who are susceptible to getting the ailment. In addition, prednisolone has the ability to inhibit the immune system, which raises the likelihood of infections and hinders the body’s ability to combat illnesses.
Prior to initiating prednisolone treatment, it is imperative to engage in a comprehensive discussion with a healthcare practitioner regarding any allergies, ongoing drugs, and pregnancy status. Additionally, it is crucial to disclose any preexisting medical disorders, such as diabetes or infections, as prednisolone has the potential to worsen these conditions.
Prednisolone carries a greater probability of inducing adverse effects, such as gastrointestinal discomfort and alterations in mood, in comparison to prednisone. Nevertheless, prednisolone is favoured in some circumstances because of its heightened potency and quicker beginning of effect.
Ultimately, prednisolone can exert notable detrimental impacts on both blood glucose levels and the immune system. Consequently, it is imperative to exercise caution and engage in a thorough discussion with a healthcare professional on personal circumstances prior to commencing this medicine.
Initial treatment’s impact on clinical outcomes
The post-treatment clinical results of nephrotic syndrome, including the influence of prolonged prednisolone treatment, are crucial. After the initial treatment, it is important to take into account the presence of frequently relapsing nephrotic syndrome (FRNS) and steroid dependence. Furthermore, the frequency of relapses experienced by each patient on an annual basis, as well as any negative consequences resulting from the treatment, are vital clinical outcomes. Prolonged administration of prednisolone may influence these results, as well as affect alterations in stature, blood pressure, corticosteroid harm, and bone mineral density.
The clinical outcomes are evaluated by measuring specific criteria such as urine protein excretion, serum albumin levels, blood pressure, and growth and bone health assessments. Assessment of these factors may entail the utilisation of laboratory tests, imaging investigations, and physical examinations. It is crucial to monitor these outcomes in order to assess the efficacy and possible negative consequences of prolonged prednisolone therapy in patients with nephrotic syndrome.
Monitoring clinical outcomes, such as relapse rates and adverse effects, is crucial following the initial therapy of nephrotic syndrome. Furthermore, it is crucial to thoroughly assess the effects of prolonged prednisolone treatment on stature, blood pressure, the harmful effects of corticosteroids, and the density of bone minerals.
Immunosuppressive therapies for the prevention of relapse
Immunosuppressive therapies have a crucial role in the management of autoimmune disorders, particularly in the prevention of relapses and regulation of the hyperactive immune system. These medicines function by inhibiting the immune system to diminish inflammation and alleviate symptoms linked to autoimmune disorders. They are frequently utilised in conjunction with other drugs to attain optimal outcomes. This article will examine the many immunosuppressive treatments frequently employed to prevent recurrence. It will delve into their mechanisms of action, potential adverse effects, and stress the significance of vigilant monitoring and effective communication with healthcare practitioners during the course of these treatments. Gaining comprehension of the function of immunosuppressive medications in the management of autoimmune disorders can offer useful understanding of the intricacies of these ailments and how they can be efficiently regulated for sustained health and well-being.
Frequently employed therapeutic approaches
Conventional and unconventional therapies are frequently employed for the treatment of mental health conditions. Commonly employed treatments encompass cognitive-behavioral therapy (CBT), a therapeutic approach that centres on the identification and modification of detrimental cognitive patterns and behaviours. Psychotherapy, a conventional method, entails engaging in dialogue with a therapist to tackle emotional and psychological difficulties. Medication management is a frequently employed approach, involving the prescription of psychiatric drugs to effectively control symptoms associated with different mental health conditions. Group therapy offers a nurturing setting for individuals to exchange experiences and get insights from others facing similar circumstances.
Alternative therapies encompass mindfulness-based approaches, such as mindfulness-based cognitive therapy (MBCT), which integrates cognitive behavioural therapy (CBT) with mindfulness practices. Art therapy and music therapy are alternative modalities that facilitate non-verbal expression and emotional processing for individuals. In addition, holistic modalities such as yoga, meditation, and acupuncture can be employed to enhance general well-being and alleviate symptoms of mental illness.
In the end, the most effective method for treating mental health may consist of a blend of conventional and unconventional therapies, customised to suit the specific requirements and preferences of the individual. Collaborating with a mental health expert is crucial in order to ascertain the optimal treatment plan tailored to an individual’s unique circumstances.
Effectiveness of Immunomodulatory Therapies in Paediatric Patients
Children diagnosed with nephrotic syndrome commonly receive a range of immunosuppressive drugs as part of their treatment regimen to effectively control their disease. Commonly employed immunosuppressive therapies encompass corticosteroids, such as prednisone, and mycophenolate.
Corticosteroids function by diminishing inflammation and inhibiting the immune system. Corticosteroids are frequently used as the initial treatment for nephrotic syndrome in children and have demonstrated high efficacy in producing remission in most cases. Nevertheless, prolonged utilisation of corticosteroids might result in several adverse consequences, such as weight gain, heightened susceptibility to infections, and decreased bone density.
Mycophenolate is an additional immunosuppressive drug used to paediatric patients diagnosed with nephrotic syndrome. It functions by suppressing the growth of immune cells, thereby diminishing inflammation in the kidneys. Mycophenolate is commonly used to paediatric patients who exhibit poor response to corticosteroids or experience frequent relapses. Evidence has demonstrated its efficacy in sustaining remission and decreasing the occurrence of relapses. Nevertheless, it can also have adverse consequences such as gastrointestinal disorders and heightened susceptibility to infections.
Although immunosuppressive medications can effectively control nephrotic syndrome in children, they also provide a risk of substantial adverse effects. The long-term consequences can differ, as certain children may achieve lasting recovery while others may necessitate continuous therapy and confront the possibility of illness advancement. Consistent surveillance and frequent communication with healthcare professionals are crucial for effectively managing the care of children diagnosed with nephrotic syndrome.
Adverse Effects of Immunomodulatory Drugs
Gastrointestinal symptoms such as diarrhoea, abdominal pain, and nausea are frequently observed as adverse effects of immunosuppressants, including mycophenolate. In addition, patients may encounter symptoms such as headaches, dizziness, and heightened vulnerability to infections. Additionally, these treatments can result in potential adverse effects such as hypertension, hepatic and renal impairments, and anaemia.
The intensity of these adverse effects may vary depending on the dosage and duration of administration. Greater doses of mycophenolate can elevate the probability of generating unpleasant responses, however prolonged usage can heighten the likelihood of suffering side effects. Individuals who are prescribed immunosuppressants should diligently monitor their symptoms and promptly inform their healthcare provider of any problems.
Ultimately, it is crucial for persons who are prescribed immunosuppressants, such as mycophenolate, to have a clear understanding of the possible adverse reactions. Individuals can effectively manage and monitor potential difficulties by comprehending the typical adverse responses and their variations, which are influenced by the dosage and length of use, and collaborating with their healthcare professional.
Incidence and Intensity of Recurrences With Immunosuppressive Therapies
Children who are newly diagnosed with idiopathic nephrotic syndrome (INS) and have a faster response to early corticosteroid medication experience varying frequencies and severities of relapses with immunosuppressive treatments, depending on the time it takes for their symptoms to improve and the length of time they get prednisolone therapy. Patients who experienced remission within 10 days of treatment with prednisolone for a duration of 8 weeks had a reduced occurrence and intensity of relapses in comparison to those who responded between 10-28 days and received prednisolone for 12-14 weeks. The previous group exhibited a reduced occurrence of regularly recurring nephrotic syndrome and a diminished need for alternative immunosuppressants. In addition, they observed a reduced frequency of relapses per patient. In contrast, the latter group exhibited a greater occurrence of relapses, more intense episodes of relapse, and a higher prevalence of frequently relapsing nephrotic syndrome. These findings emphasise the significance of determining the most effective length of prednisolone treatment by considering the time it takes for remission to occur. This will lead to improved management of relapses in children with INS. Additional investigation is required to examine the enduring consequences of these distinct therapeutic methods on the frequency and severity of relapses.
